Responsum for CKD
{{user.displayName ? user.displayName : user.userName}}
{{ user.userType }}

Only a quarter of kidney transplant recipients know that their risk of skin cancer increases post-transplant. Find out why and how to protect your skin.
Skin cancer is one of the most common types of cancer in people who have undergone a kidney transplant. This discovery was made through research that looked at the effect of immunosuppressive drugs on one’s overall health. The study’s findings showed that this type of medication, which is prescribed to protect transplanted organs, can weaken your immune response.
Experts have revealed that only about 25% of transplant recipients know that they are at increased risk for developing skin cancer, so increased awareness is vital. Find out more about the link between kidney transplants and skin cancer and how to protect your skin.*
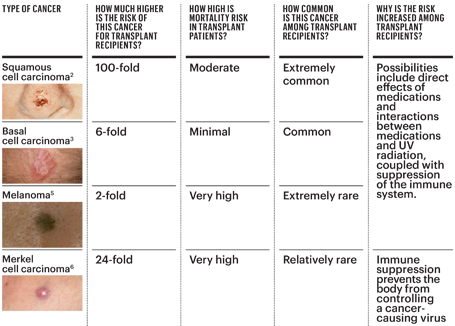
Squamous cell carcinoma (SCC) is a type of skin cancer that has been found in transplant patients. In fact, it is 65 times more common in people with transplants than in people without the procedure.
Basal cell carcinoma has also been found to be more common in transplant recipients, with melanoma and Merkel cell carcinoma (MCC) being even less common. MCC and SCC are more likely to spread throughout the body in transplant patients compared with the general population, so understanding what each form of cancer looks like is essential.
While all transplant patients are at risk for skin cancer, it’s also important to keep in mind the other factors that indicate a higher risk.
These risk factors include:
Skin cancer does not usually develop immediately after transplantation; it typically occurs three to seven years post-transplant. This can often be attributed to long-term medication adherence and high doses of immunosuppressive drugs.
Kidney transplant patients who spend many healthy, active years on immunosuppressive medications need to be especially aware of ways to prevent skin cancer to have ample time to take steps to protect their skin early on.
There are three main ways you can protect your skin to help avoid a skin cancer diagnosis:
No matter the time of year, begin a regular sunscreen application regimen with a Sun Protection Factor (SPF) of at least 30 and a “broad spectrum” label, which protects you from UVA and UVB rays. Apply your sunscreen 15 to 20 minutes before going outside, and reapply every two hours if you continue to stay outdoors.
It’s important to note that a higher SPF rating does not mean that the sunscreen will last longer. Two hours is a rule of thumb for all SPFs. In addition to SPF, sun-protective clothing and hats can also reduce your exposure to harmful rays. This is especially useful when you’re spending time around water, sand, and snow, on which the sun reflects strongly.
You should also seek shade between the hours of 10 a.m. and 4 p.m.
You should examine your skin once a month for any abnormalities. You will often be the first person to notice a new or changing skin lesion, so it’s important to check at least once a week. Look at all areas, including your scalp, hands, feet, genitals, and even your nails, as skin cancer can even occur in areas that are not always exposed to the sun.
Consider having a partner, family member, or friend look at areas that are difficult to examine. You must urgently see a doctor if you see red or scaly areas, bleeding or scabbed spots, painful lesions, or changing moles.
The four aforementioned types of skin cancer might look like the following:
Even if you do not notice any areas of concern on your skin, have a dermatologist check your skin at least once a year. Your doctor is trained to find skin cancers and precancerous lesions before they become visible to you. This will allow you to act early and prevent them from worsening. Patients with multiple skin cancers may need to see their dermatologist more frequently, possibly even monthly.
For high-risk patients, your dermatologist may prescribe medications and treatments that can be used to manage precancers and slow the progression of skin cancer development. “The oral retinoid acitretin can prevent SCC in transplant recipients, and new data suggest that nicotinamide (a variant of vitamin B3) may also be protective in patients who have already had SCC,” according to the Skin Cancer Foundation.
While you can take preventive steps post-transplantation to decrease your risk of a future skin cancer diagnosis, you can also find solace in the fact that when skin cancer is found early, it can often be easily treated.
Additional information can be found on the Skin Cancer Foundation website.
*Nunley, K. S. (2020, June 5). Protect the Skin You’re In. National Kidney Foundation. https://www.kidney.org/transplantation/transaction/TC/Summer13/Protect-the-Skin-Youre-In
Source: {{articlecontent.article.sourceName}}
Receive daily updated expert-reviewed article summaries. Everything you need to know from discoveries, treatments, and living tips!
Already a Responsum member?
Available for Apple iOS and Android
Add Comments
Cancel