Responsum for CKD
{{user.displayName ? user.displayName : user.userName}}
{{ user.userType }}

Learn some basics about the causes of and treatments for chronic kidney disease.
Chronic kidney disease (CKD) is a prevalent yet too-often undetected condition affecting tens of millions of Americans. Its silent progression renders many unaware until irreversible damage has occurred, necessitating intensive interventions like dialysis or kidney transplants. Here, Dr. Randy Luciano, a nephrologist at Yale Medicine, shares insights on CKD’s nuances and effective management.*
CKD is defined by a gradual decline in kidney function over a minimum of three months, though it’s frequently not detected for several years, even decades. This decline leads to the accumulation of toxins and fluids in the body. Diabetes and high blood pressure are the two primary culprits, and if left unmanaged they will continue exacerbating the kidney damage.
Other contributors include obesity and genetic predisposition. Polycystic kidney disease is one form of CKD that a person is born with, for which there is currently no cure. Understanding CKD’s multifaceted origins is pivotal in its early detection and treatment.
Certain demographics face heightened susceptibility to CKD, such as:
Racial and socioeconomic disparities underscore the complex interplay of:
Genetic testing offers a proactive approach for high-risk populations, enabling tailored interventions to mitigate CKD progression.
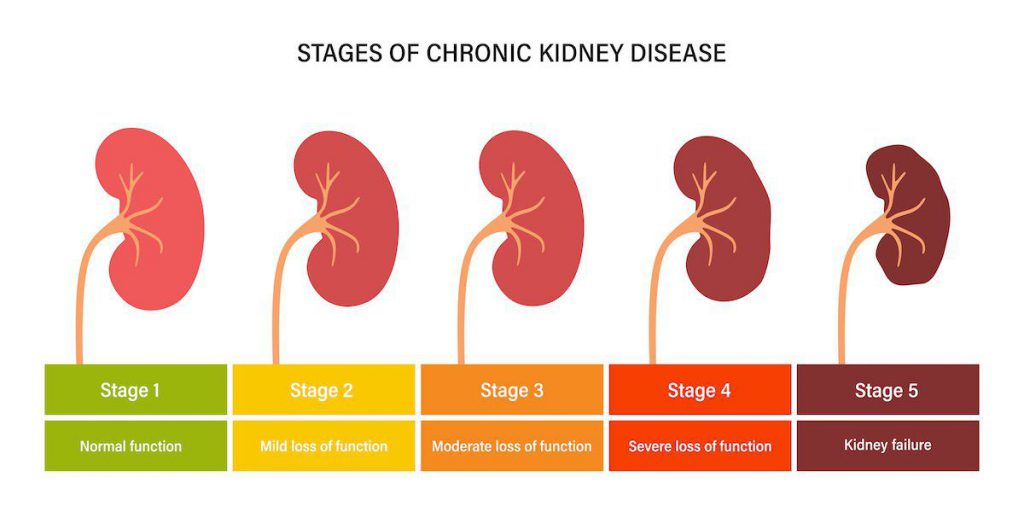
Early diagnosis hinges on routine blood and urine tests, gauging kidney function and detecting proteinuria (excessive protein levels in your urine). Determining your stage of CKD involves assessing glomerular filtration rates (GFR)–the percentage of your remaining kidney function–and identifying associated symptoms. The progressive nature of CKD underscores the importance of timely interventions, as treatment efficacy varies across stages.
In general, the stages of CKD by estimate GFR (eGFR) are:
Stage 1: eGFR is equal to or greater than 90 but less than 100
Stage 2: eGFR is 60 to 89
Stage 3a: eGFR is 45 to 59
Stage 3b: eGFR is 30 to 44
Stage 4: eGFR is 15 to 29
Stage 5: eGFR is less than 15
Tailored treatment usually involves dietary and other lifestyle adjustments, such as quitting smoking and getting sufficient sleep, alongside pharmacological interventions to address underlying causes like diabetes and hypertension.
Emerging medications like SGLT-2 inhibitors and GLP-1 receptor agonists offer promising avenues for slowing CKD progression.
While not all CKD cases culminate in end-stage kidney disease (ESKD), dialysis and transplantation are vital treatment models for those affected. Depending on your individual situation, various dialysis options provide flexibility and convenience, enhancing and prolonging patients’ quality of life. Kidney transplantation remains the gold standard, offering improved outcomes and reducing reliance on dialysis.
Many of the lifestyle habits used to prevent CKD progression can also be used to help prevent it from starting in the first place. An effective, holistic approach to kidney health encompasses:
By fostering kidney awareness and proactive management, you can mitigate the impact of CKD and optimize your long-term health.
*Katella, K. (2024, April 24). Why Is Chronic Kidney Disease on the Rise? 6 Things to Know. Yale Medicine.
https://www.yalemedicine.org/news/why-is-chronic-kidney-disease-on-the-rise
Responsum Health closely vets all sources to ensure that we always provide you with high-quality, reliable information. We do not, however, endorse or recommend any specific providers, treatments, or products, and the use of a given source does not imply an endorsement of any provider, treatment, medication, or procedure discussed within.
Source: {{articlecontent.article.sourceName}}
Receive daily updated expert-reviewed article summaries. Everything you need to know from discoveries, treatments, and living tips!
Already a Responsum member?
Available for Apple iOS and Android
Add Comments
Cancel